Trauma to the neck can cause acute pain. Chronic pain and dysfunction from such injury is called “whiplash-associated disorder” (WAD). WAD is a very common complication to people who were involved in a Motor Vehicle Collision. The Quebec Task Force [QTF] classified WAD severity. The key points of QTF are as follows:
• Whiplash is the most common injury associated with motor vehicle accidents and a major cause of disability and litigation.
• Whiplash-associated disorders (WAD) can be classified by the severity of signs and symptoms from Grade 0 to 4.
• Patients usually complain of neck pain and stiffness in the acute phase, with the majority recovering within 3 months.
• Depression, anxiety, and mood disorders are common in patients with chronic whiplash.
• Reassurance, early mobilization, simple analgesic, and physiotherapy are recommended in acute whiplash (WAD I–III).
• In chronic WAD, multidisciplinary pain clinic referral followed by cognitive behavioural therapy and cervical radiofrequency neurotomy plays an important role.
Although there are many treatment approaches to a whiplash injury, one study was able to specifically demonstrate the efficacy of treatment using intramuscular stimulation therapy.
In this study Forty-three (43) people accepted intramuscular stimulation therapy. They had pain and abnormal physical signs such as allodynia, trophedema, muscle knots, and limited range of motion. With treatment, twenty-nine achieved long-term improvement.
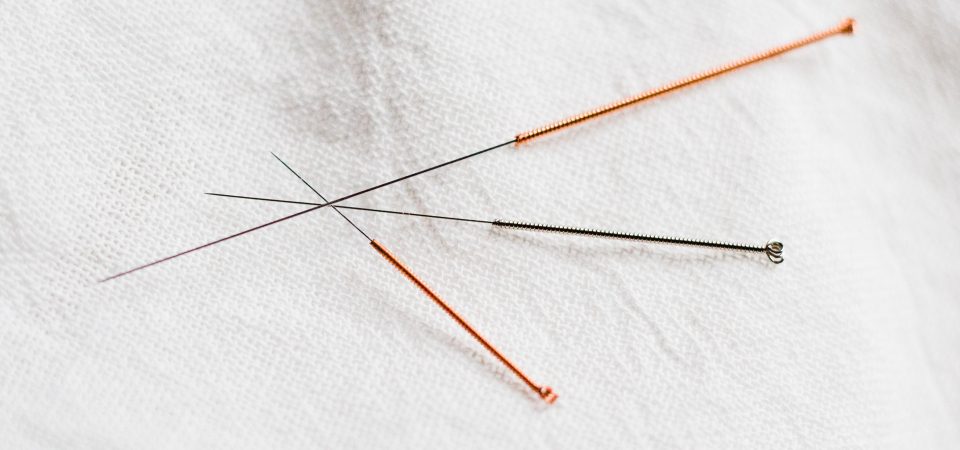
In an IMS treatment, when the needle enters, the muscle will ‘grab’ the needle and a deep, cramping sensation is felt. Once the muscle grabs it then typically will ‘reset’ itself and begin to relax. When the tight muscle relaxes, a decrease in pain typically follows. IMS is now being recognized and used by physiotherapists and doctors around the world to treat chronic pain of musculoskeletal origin.
Conclusion
The whiplash disorder symptoms were due to abnormal function of the central nervous system. Most subjects improved subjectively and their abnormal physical signs resolved. Such direct clinical evidence of benefit is clearly meaningful.